Ultrasound Case Study
Anterior elbow pain: A case of partial tear of the distal biceps tendon
Stuart Wildman, Extended Scope Physiotherapist and MSK Sonographer
On examination, there was no obvious deformity. There was full passive range of the elbow with no pain. There was no visible effusion. He had reasonable power, which was painful although slightly weaker than his asymptomatic side. It was possible to palpate the biceps tendon with elbow in full extension, although this was tender.
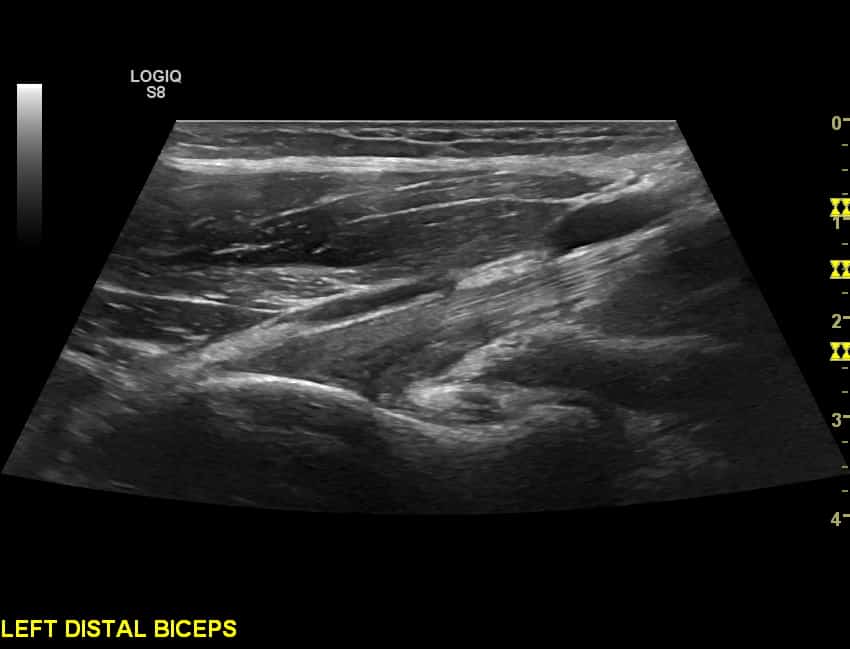
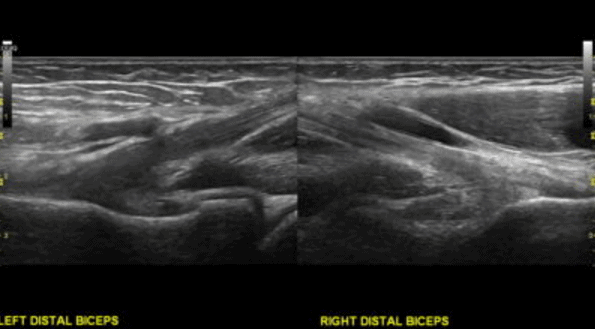
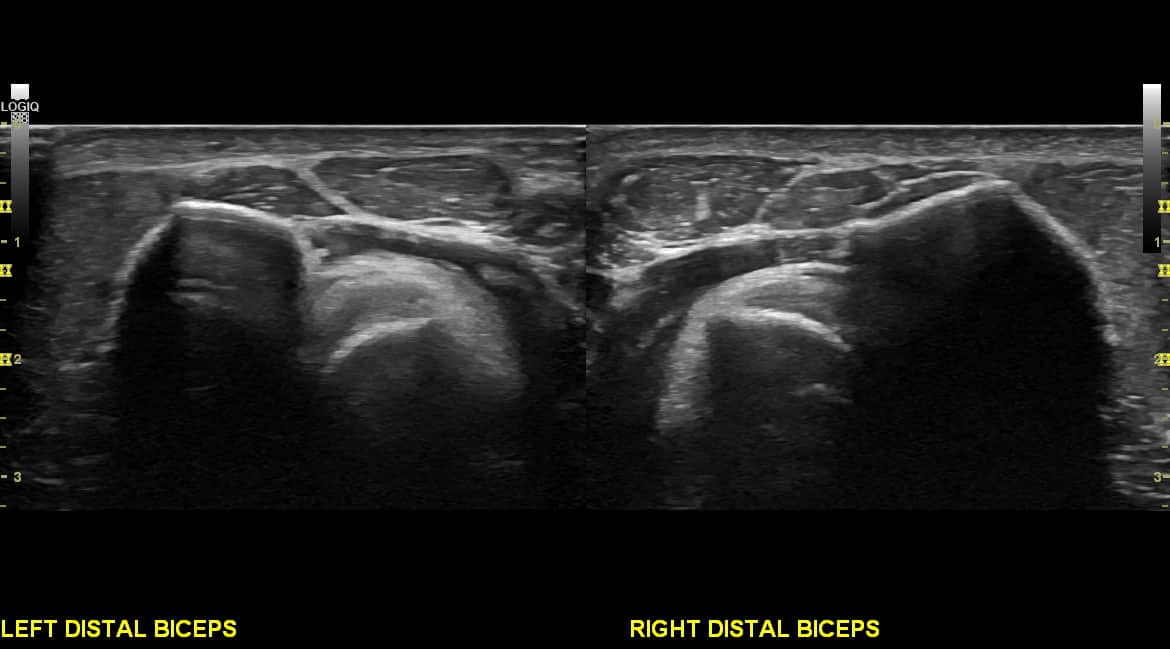
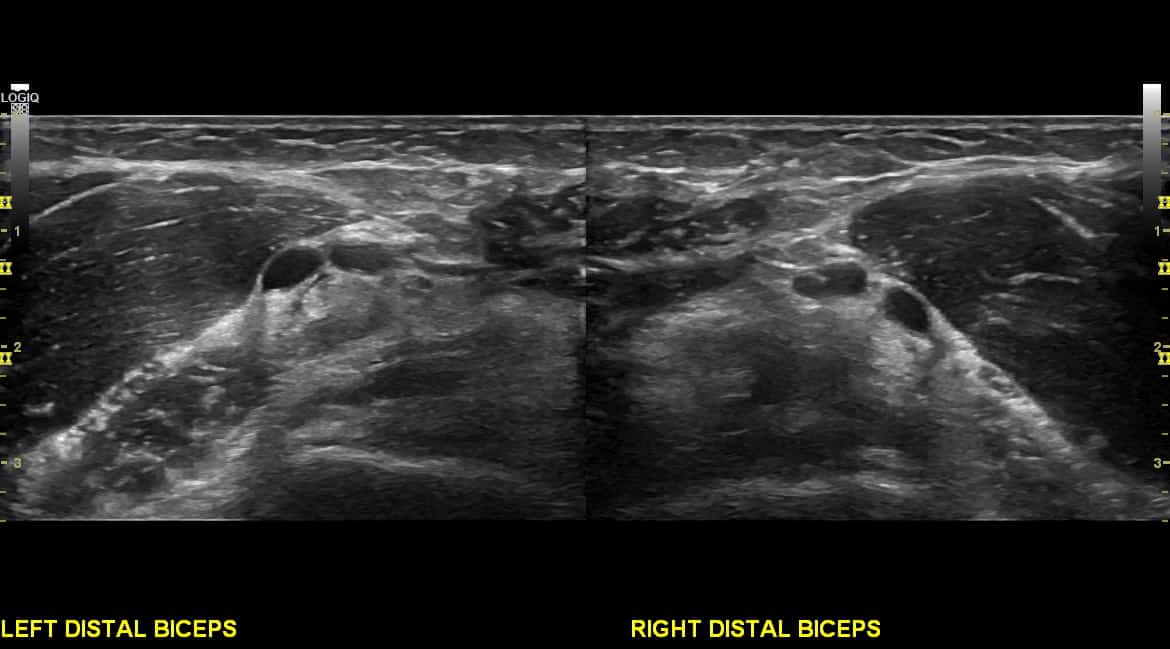
On ultrasound, the images to the right were encountered. It is difficult to always correlate the very distal insertion on short axis and longitudinal view as this is a challenging tendon to interrogate. There was a distinct difference in the echotexture of the distal tendon in comparison to the asymptomatic side.
Differential diagnosis:
- Complete rupture of the biceps tendon
- Partial thickness tear of the biceps tendon
Final diagnosis: Ultrasound appearances suggestive of a partial tear of the distal biceps tendon, with loss of the normal echotexture in the deeper aspects of the tendon measuring L1.63cmx 0.60cm.
Further imaging was advised and the diagnosis was confirmed later on MRI with similar measurements to the longitudinal view on ultrasound.
Discussion
Distal biceps tears tend to occur in middle aged men and are usually related to trauma.
Tears of the distal insertion of the biceps are less common than the proximal tears of the long head of biceps (Lobo et al, 2013). Clinically, complete ruptures of the distal biceps insertion are easily diagnosed, with significant loss of power, palpable defect in the antecubital fossa and noticeable functional difficulties. Partial thickness tears are more challenging to highlight clinically (Miller & Adler, 2000), with a varied presentation and diffuse pain reporting. MRI has been shown to be reliable for evaluating the distal biceps, however, ultrasound is increasingly used as it is more accessible, cheaper and can be used dynamically (Lobo et al, 2013). There is however a lack of research comparing reports and surgical findings.
Ultrasound has been shown to differentiate between complete and partial tear with 95% sensitivity , 71% specificity and 91% accuracy. It is however a challenging structure to visualise and difficult to correlate short axis images with long axis views.
References


What kind of treatment did he have after this diagnose?