Ultrasound Case Study
Pretibial ganglion following ACL reconstruction
Stuart Wildman, Extended Scope Physiotherapist and MSK Sonographer
This interesting case was referred for assessment after the patient had experienced 6 months of anterior knee pain, with a background history of an Anterior Cruciate Ligament repair. The patient was in their 20’s and presented with soreness in the region of the tibial tuberosity. They could not recall any recent trauma, and had no initial complications following the surgery. They reported no episodes of locking , giving way or instability. They did recall an occasional smaller area of swelling appearing on the anterior shin over recent months.
On examination, there was nothing of note on observation with no wasting, swelling or deformity. The scars following the ACL reconstruction were visible. There was full knee range of movement. There was some localised tenderness medial to the tibial tuberosity, directly where the ACL scar was. The patient had previously had an x-ray which reported the ACL repair but nothing else of note. The x-ray image can be seen to the right.
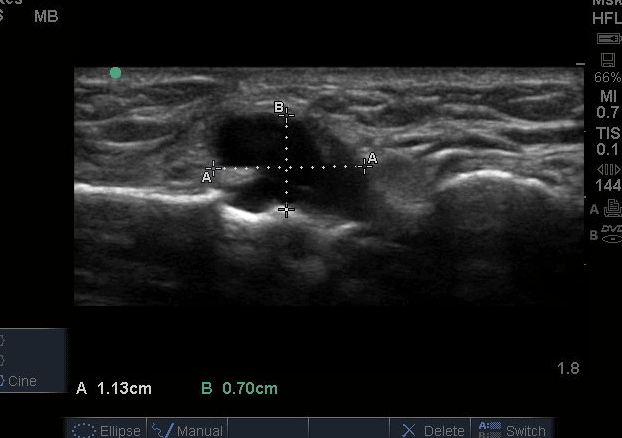
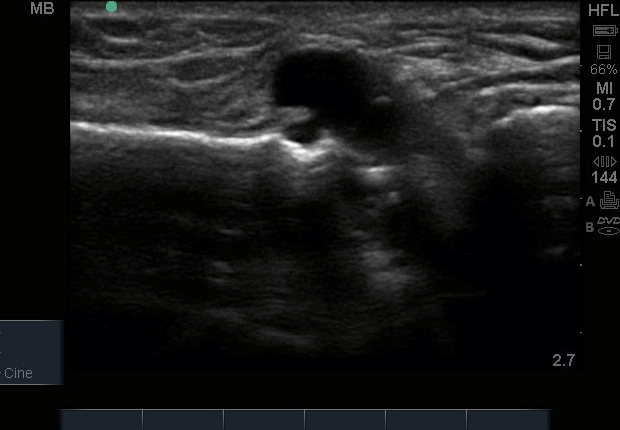
With diagnostic MSK ultrasound (see images below and in gallery), the patellar tendon and insertion onto the tibial tuberosity were intact. There was no evidence of deep infrapatellar bursitis. There was an anechoic, non-compressible lesion medial to the tibial tuberosity (Figure 2 and 3), which appeared to communicate with the cortex of the tibia in the region of the ACL scar. There was no vascularity visible. It was not compressible and there appeared to be a clear line of communication with the cortical irregularity. The lesion was painful under pressure from the probe, reproducing the patients symptoms.
A video of the finding can be seen below, highlighting the proximity to the patella tendon.
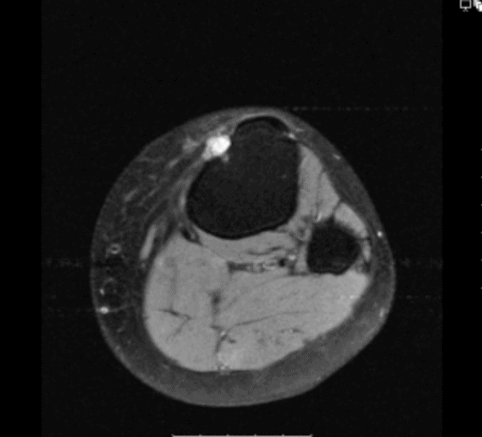
An MRI was requested to image this lesion further, and was reported as normal. On reviewing the images, a fluid collection was visible on the anterior tibia which correlated with the ultrasound findings. The patient has now been referred for an Orthopaedic opinion of the pretibial ganglion. The access to diagnostic ultrasound in clinic dramatically accelerated this patients care, as the physical examination overall was unremarkable with only localised tenderness near the tibial tuberosity. The ultrasound findings provided more information, that correlated with the clinical presentation. Utilising the ultrasound and clinical findings also enabled a critical evaluation of the MRI.


0 Comments