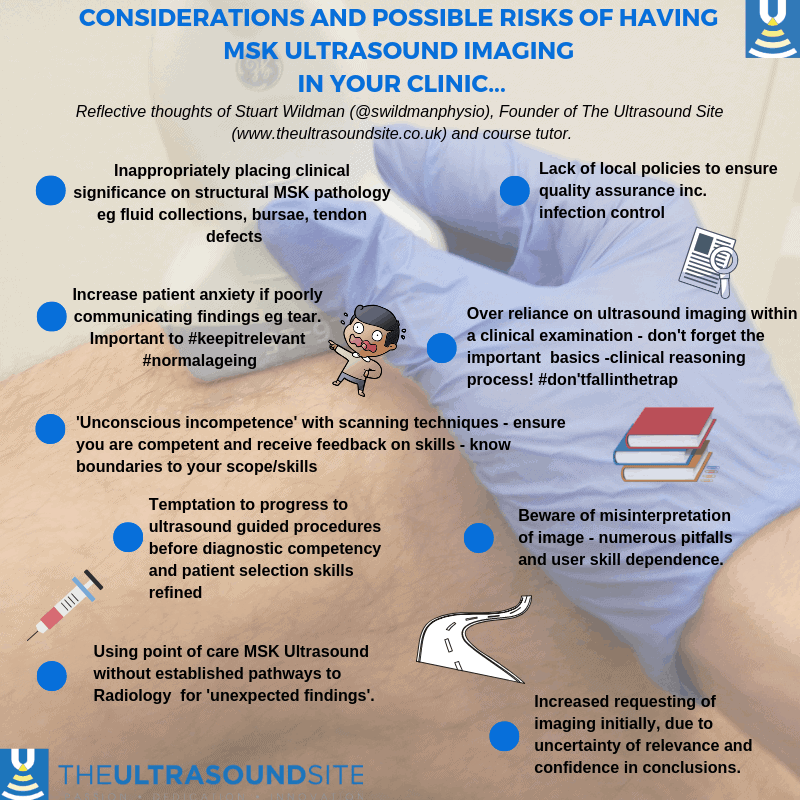
I thought I would develop a more extensive blog on the topic of the considerations and possible risks of having MSK ultrasound imaging in your clinic. This is a challenging skill to integrate into your practice. I sometimes feel that this maybe does not get the recognition it should in and amongst all the excitement of this expanding area. I also received a fantastic amount of feedback after releasing an infographic on this topic 6 months ago on social media. So I thought it might be helpful to elaborate on the individual points that are raised within that infographic to hopefully provide a more in-depth learning experience for clinicians looking to integrate this skill into their practice.
I will explore each of the points raised in the infographic image in more depth, and look forward to your feedback and discussion. This is certainly not exhaustive, but highlights some of the key considerations.
Inappropriately placing clinical significance to structural MSK pathology
We are increasingly aware of the prevalence of asymptomatic pathological findings on musculoskeletal imaging, whether that be relating to the spine, peripheral joints or specific musculoskeletal structures. One of the risks of using ultrasound in your clinic is that you can simplify the clinical reasoning process, placing too much significance on sonographic findings. For me, the key issue here is ensuring that those using ultrasound in point of care clinics have a good level of clinical experience and are also reflective practitioners. Should we be encouraging professional bodies to stipulate a minimum level of experience before using ultrasound in practice? Difficult one to answer!. We should certainly be encouraging all clinicians using ultrasound to be reflective on its impact on patient management – the ‘So what?’ response to clinical and imaging findings comes to mind! More discussion points on this topic can be found here.
Lack of local clinical governance policies
With the rapid growth of this modality into point of care environments it is vital that local policies are developed to ensure a high standard of practice. These may range from infection control policies to how to handle unexpected findings. Please read our other blog on standards of ultrasound practice for further information – due to be released soon! This is a topic we cover in detail on our PG Cert MSK ultrasound program with Brunel University London
Increased patient anxiety
With ultrasound being primarily focussed on the evaluation of structural musculoskeletal change it is important that clinicians are aware of the prevalence of asymptomatic findings and normal age related change. We are also increasingly aware of the impact that the language medical and allied health professionals use can impact the outcomes to treatment. The ability to communicate findings confidently and appropriately takes experience and skill, this should not be underestimated. Normalising age related structural change can often be as powerful as diagnosing a clinically relevant structural problem. It is the ability of the clinician to ‘stitch’ the sonographic and clinical findings together in an understandable way that really enables ultrasound to shine in this environment.
Over reliance on MSK ultrasound
This echoes the points raised earlier, but I think the key message here is that ultrasound sits as one of the building blocks within the clinical reasoning process. It does not provide a quick answer to increasingly challenging clinical scenarios that we encounter on a daily basis.It plays a different role for different patients.
Unconscious incompetence
One of the most regularly talked about topics of musculoskeletal ultrasound is how it is a very user dependent imaging modality. This could actually be said of a number of imaging modalities such as MRI, X-ray and CT which ultimately are all user dependent to an extent as an image is reported by a human in a subjective way which is open to error. The difficulty ultrasound faces is that alongside the reporting process and the image interpretation, there is a requirement for a significant level of motor skill to generate an accurate image initially. The image interpretation is dependent on the image quality essentially. This provides the opportunity for unconscious incompetence around the ability to visualise certain structures and make judgements. Again, be a reflective and responsible clinician – you should know the limits of your skills and the scope of practice. It is also important to understand where ultrasound does play a role but also when other imaging is a much more suitable.
Progression to MSK ultrasound guided procedures
As a result of the growth of access to musculoskeletal ultrasound there has also been a growth of interest around ultrasound guided musculoskeletal injections. We have written a separate blog regarding this and the need for caution and consideration when making this step. The key issue here is that there needs to be a level of competency using diagnostic ultrasound for musculoskeletal conditions prior to progression to performing guided procedures. It is important that the clinician can interpret a sonographic image competently prior to the decision making of when to inject. As ultrasound is made up of greyscale appearances many structures can appear very similar when viewed by a novice e.g. Artery, vein, anisotropy of a tendon and distended bursa.
Misinterpretation of a sonographic image
As we mentioned several times in this blog, there is a skill required to generate a high quality sonographic image. Within MSK ultrasound you often having to visualise structures which have tortuous and complex routes. This requires excellent anatomical knowledge and the ability to manipulate your ultrasound probe to visualise structures accurately. Without this, images can look very different and inappropriate clinical conclusions can be made. One key artefact that is often mentioned is Anisotropy. We have written a full article on Anisotropy, which can be accessed here.
Unexpected findings
As with any imaging modality it is possible at times to come across unexpected findings. When utilising ultrasound in clinic you start to become aware of the limitations of your clinical examination and that other pathologies can occur which were not expect. It is imperative that if you are using ultrasound in clinics you should have established pathways to a radiology setting to handle unexpected or serious pathology findings. It is strongly advised that you have a local policy outlining this process to protect yourself from a medicolegal perspective.
Increased requesting of other imaging
It is important to acknowledge that when a clinician starts to utilise diagnostic MSK ultrasound in clinic they may initially request more investigations as part of the learning process. This may be in part to verify their findings on ultrasound but also as with any new skill that is acquired it takes some time to establish confidence in your new abilities to visualise structures. This is why it is vital that anyone utilising ultrasound and training in it, has access to high quality mentoring and peer support. Case discussion and reflection are key.