Ultrasound Case Study
Patella tendinopathy and non-union of the ossification centres
Dr Matthieu Sailly (@MedecinsDuSport) Sports Medicine Physician, Switzerland
Following on from the recent case I posted on patellar tendinopathy and the role of diagostic MSK Ultrasound, Dr Matthieu Sailly, Sports Medicine Physician at Centre Synergie Medical, Lausanne in Switzerland got in touch and has contributed the following clinical thoughts on patellar tendinopathy and non-union of ossification centres. With a focus on the potential sequel of complaints that may arise following non union of the ossification centre.
Tibial tuberosity
Osgood Schlatter disease (OSD) may lead to chronic symptoms in 5 to 12% of the cases depending the literature (1). Distal patellar tendinopathy is not so frequent. This condition is often associated with bone graft harvest following ACL reconstruction or non-union of the ossification centre.
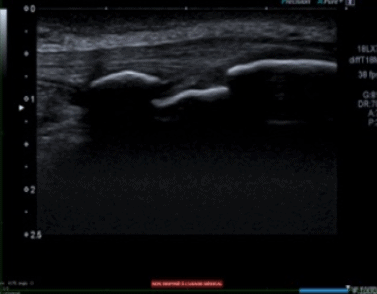
During the endochondral ossification, a part of the ossification center does not fuse properly leading to a definitive non-union. This an example from a young talented basketball player (Figure 1) . He is 18 yo and has a past history of OSD. He is currently symptom free because this is the off season. He reports some pain during kneeling or during direct trauma on this area.
Base of patella
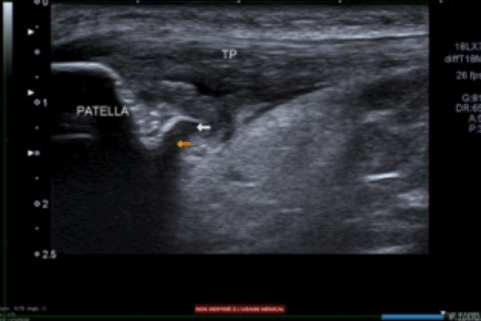
In some cases, proximal patellar tendinopathies are associated with local impingement during knee flexion due to an “aggressive tip of patella” (2). This is illustrated below.
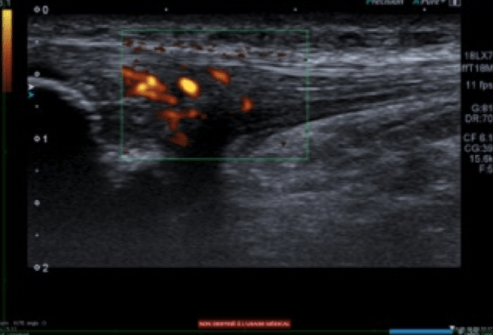
This deformity of the tip of the patella may be related to the non-union of the ossification centre. This is an example of ballet dancer 19 yo. She complained of a jumper’s knee for 3 months, and was referred to our clinic. The ultrasound scan in clinic demonstrated an ossification defect visible at the deep portion of the tendon that created impingement during knee flexion. The patellar tendon has a hypoechoic signal, loss of fibrillar aspect, Doppler signal. Interestingly the superficial layer of the tendon looks normal.
During follow-up the deep portion of the tendon remained the same despite symptoms improving.
Overall, apophysitis is a common pathology this is often underestimated. Additional studies should look at the long-term consequences and the relation with some insertional tendinopathy during adulthood.
1) Rosenberg ZS, Kawelblum M, Cheung YY, Beltran J, Lehman WB, Grant AD. Osgood-Schlatter lesion: fracture or tendinitis? Scintigraphic, CT, and MR imaging features. 1992 Dec;185(3):853-8
(2) Johnson DP, Wakeley CJ, Watt I. Magnetic resonance imaging of patellar tendonitis. Journal of Bone Joint Surgery (Br) 1996 May;78(3):452-7
A further article of interest may be this full text from Dr Sailly and colleagues..
For further thoughts on patellar tendinopathy and the use of MSK Ultrasound and MRI view a different article HERE
0 Comments