Ultrasound Case Study
Achilles tendinopathy
Peter Gettings, Physiotherapist and MSK Sonographer
It is well documented that musculoskeletal ultrasound is an important imaging modality when considering Achilles’ tendon pathology. This very useful article by Klauser et al (2012) used a Delphi-based consensus to come up with clinical indications for musculoskeletal ultrasound. Using the criteria below they concluded that, when assessing tendons and soft tissue at the ankle, MSKUS was the first choice technique and in many cases this was backed up with Level A evidence.
Grade 0: MSKUS not indicated
Grade 1: MSKUS indicated if other imaging techniques are not appropriate
Grade 2: MSKUS indication equivalent to other imaging investigations (other investigations might provide significant information)
Grade 3: MSKUS is first choice level technique (other investigations rarely provide more information)
Level A: Consistent randomised controlled clinical trial, cohort study, all or none clinical decision rules validated in different populations.
Level B: Consistent retrospective cohort, exploratory cohort, outcomes research, case–control study; or extrapolations from level A studies.
Level C: Case-series study or extrapolations from level B studies.
Level D: Expert opinion without explicit critical appraisal, or based on physiology, bench research of first principles.
The patient reported a long history of Achilles pain that had been present for many years but had worsened recently for no apparent reason. The study from de Jonge et al (2011) reported that the incidence rate of Achilles tendinopathy was 1.85 per 1,000 patients.
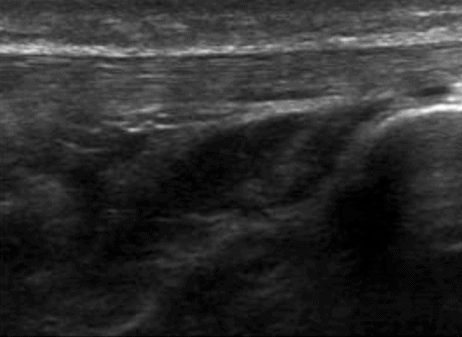
Normal sonographic appearance of a tendon is discussed here in this 2012 paper by Lee. Generally, a healthy tendon will look something like figure 1 below with orientation of the fibres along the long axis of the tendon with tightly spaced echogenic parallel lines in a fibrillar pattern.
On assessment the patient had visible Haglund’s deformities (Figure 2) and this paper from van Dijk et al, 2011, is useful as it has terminology for Achilles related disorders. The scan was carried out with the patient in prone following the ESSR guidelines for an MSKUS scan of the ankle. The Achilles’ tendon was significantly thickened, measuring 10mm x 24mm with hypoechoic areas throughout (Figure 3). The normal mean values for an Achilles’ tendon are 4.3mm x 14.3mm. This gentleman had significant vascularity within the tendon (figures 4 & 5) but when looking at the assessment of vascular activity within tendons this study from Tol et al (2012) reminds us that detection of neovessels offers little information in relation to symptoms,diagnosis or prognosis of the condition.
During the scan I discussed symptom management and he reported that he found that remaining active seemed to help reduce his pain and that he was keen to be able to carry on with his regular daily activities. I encouraged him to do this within limits of pain as suggested by Silbernagel et al in the 2007 article. The patient is due for review with his therapist next week and my post scan recommendation was to commence a pain monitored loading regime.
For some further reading I would highly recommend this paper from Patil and Dasgupta (2012) as it is an excellent summary of how diagnostic ultrasound can be used in the assessment of musculoskeletal diseases. No MSKUS writing would be complete without this from Schmidt et al (2004) which is an indispensable guide to standard reference values for most MSK common structures.


0 Comments