Ultrasound in Rheumatology: Gout and ultrasound
Dr Qasim Akram, Consultant Rheumatologist
Gout (or monosodium urate [MSU] crystal deposition disease) is a crystal arthritis due to an oversaturation of uric acid (0.21-0.42mmol/mol) which accumulates in the blood and then is deposited within joints most commonly, but also tendons, to cause a gouty arthritis.
It is the commonest form of inflammatory arthritis in the UK and affects men more so than women and is rare in young age.
Typical risk factors for this are a high alcohol intake (including binge drinking), excess red meat, fructose containing drinks, metabolic syndrome and a high BMI. Others include the use of diuretics, dehydration and renal failure.
Pathophysiology
Uric acid is a breakdown of purines that are found naturally in the body and also through diet. Gout is usually caused by a build of uric acid either as a result of overproduction or underexcretion by the kidneys. An excessive alcohol intake or a high intake of red meat can cause an overproduction of purines. A high BMI, metabolic syndrome and fructose containing drugs do the same. Kidney failure result in an underexcretion of gout. Diuretics act on the kidneys to cause an underexcretion of uric acid.
Clinical Presentation
Patients with a typical flare of gout tend to present either with a sudden onset of a monoarthritis usually starting in the 1st MTPJ. This is known as podagra. Symptoms may also progress to involve other joints of the lower extremities such as feet, ankles and knees. The hands/wrist can also be involved and mimic a rheumatoid arthritis especially in a polyarticular pattern.
Frequent and untreated episodes can lead to the development of a chronic gouty arthritis (with erosive and destructive changes) and a tophaceous gout classically in the helix of the ears. A careful inspection of this is mandatory!
Osteoarthritic changes in interphalangeal joints (Heberden’s and Bouchard’s nodes) may predispose these joints to develop coexisting gout particularly in older individuals with chronic kidney disease or in those receiving diuretic therapy.
Other less common sites tendon to be the axial spine and flexor tendons.
Gout flares tend to resolve spontaneously and gradually over the course of a few days to weeks.
Laboratory analysis usually shows that the Inflammatory markers are usually elevated in a flare up of gout. Serum urate can also be elevated but in a flare, it is not diagnostic. It is of more value 2-3 weeks after a gout flare up resolves and to help guide treatment changes.
X-rays of the affected joints can show subcortical bone cysts that are suggestive of gouty tophi or erosions. More specific gouty lesions are juxta-articular erosions and tophi.
The gold standard diagnostic test is to obtain a synovial fluid biopsy. Laboratory analysis typically shows monosodium urate crystals that are needle shaped and negatively birefringent under polarised microscopy.
Treatment is usually aimed at lowering this urate burden through medications to prevent gouty flares and also the progression to a chronic arthritis. During an acute attack anti-inflammatories, colchicine and steroids are needed.
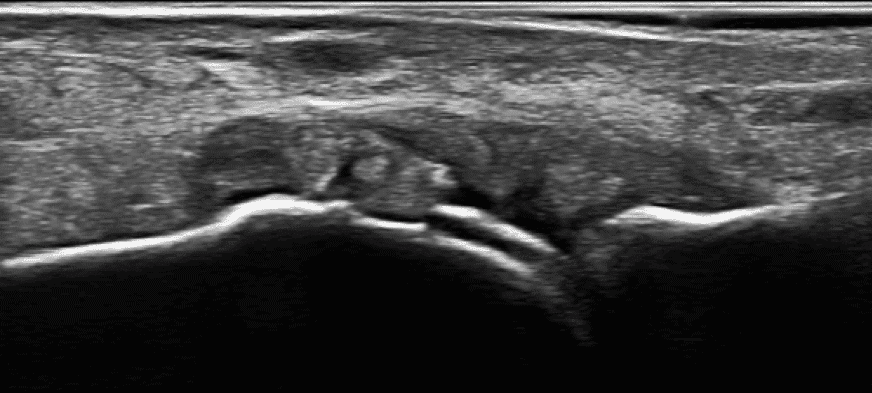
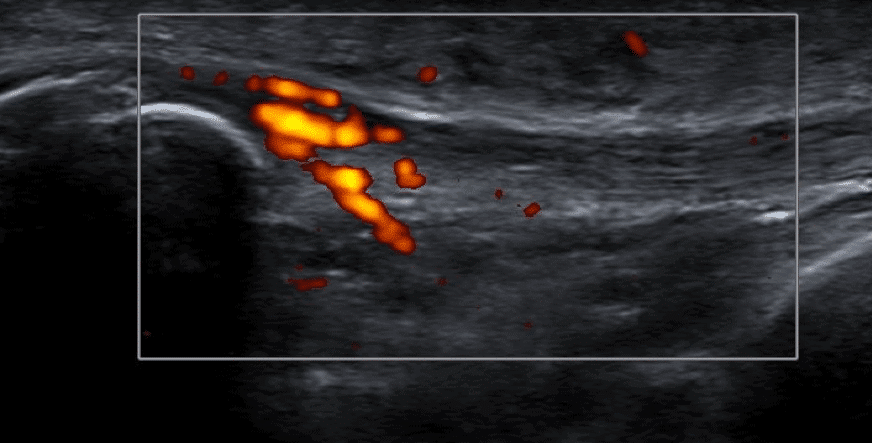
Ultrasound in Gout
Ultrasound findings can strongly and independently support the diagnosis of gout and may be useful in the early detection and monitoring of treatments. Important features are the double contour sign which appears as a hyperechoic linear density on the surface of the articular cartilage and is highly specific. Tophaceous deposits, in joints or tendons, are represented by a ‘sugar lump’ appearance. Ultrasound can also be used to obtain synovial fluid for analysis in this context.
Commonest sites include the 1st MTPJs, the femoral articular cartilage, elbow joint articular surface.
References
Clunie G et al. Oxford Handbook of Rheumatology. 4th Oxford University Press 2018.
0 Comments