Ultrasound in Rheumatology: Pseudogout
Dr Qasim Akram, Consultant Rheumatologist
Calcium pyrophosphate crystal deposition (CPPD) disease is the spectrum of conditions causes by CPP deposition. This included an acute inflammatory arthritis, degenerative chronic arthropathies, or a radiographic cartilage calcification.
Precipitation of crystals of calcium pyrophosphate dihydrate (CPP) in connective tissues may be associated with several of these clinical syndromes but is sometimes asymptomatic.
Pathophysiology,
Usually CPPD tends to affect late, patients in their middle age or the elderly. Men and women are affected equally.
Most cases can be idiopathic. However, it can also be brought about by injury, severe illness or major surgery. Metabolic causes include hyperparathyroidism, hemochromatosis and hypomagnesaemia, hypophosphatasia, and familial hypocalciuric hypercalcemia.
CPP crystals that are embedded within tissues i.e. tendons or cartilage don’t cause any problems. Crystal shedding is the process of movement of these crystals to exposed sites and contact with the immune defence via the bloodstream which is responsible for the acute inflammatory joint symptoms.
Pseudogout is the term to describe acute attacks of CPPD-induced synovitis, which clinically resemble acute attacks of (monosodium urate) gout. However, the majority of individuals with CPPD never experience such episodes.
Chondrocalcinosis refers to radiographic calcification in hyaline and/or fibrocartilage. It is commonly present in patients with CPP crystal deposition disease but is neither absolutely specific for CPPD nor universal among affected patients.
Clinical Presentation
Acute CPP crystal arthritis is characterized by self-limited acute attacks of arthritis involving only one or several extremity joints. The traditional term pseudogout underlines the usually close resemblance of these attacks to those of urate gout, in the accompanying symptoms and signs of severe acute inflammation (intense pain, redness, warmth, swelling, and joint disability). Common joints are the knees, wrists, elbows and shoulders.
Sometimes a chronic form of CPPD can exist and resemble rheumatoid arthritis. This is usually due to recurrent episodes of an acute flare that is not adequately treated which progresses. This presentation of CPPD disease resembles RA in several respects, including the presence of significant morning stiffness, fatigue, synovial thickening, localized oedema, and restricted joint motion due either to active inflammation or to flexion contracture.
The gold standard for diagnosis is synovial fluid analysis. This demonstrates characteristic positively birefringent CPP crystals (seen by polarized light microscopy).
X rays show CPPD as calcification or linear densities in articular cartilage (fibrocartilage and/or hyaline cartilage) and, with lesser frequency, in ligaments, tendons, synovia, bursae, and joint capsules. Commonly affected fibrocartilages in CPPD disease are the menisci of the knee (usually bilaterally), the symphysis pubis, the triangular fibrocartilage of the wrist joints, and the glenoid and acetabular labrum.
Typical US findings
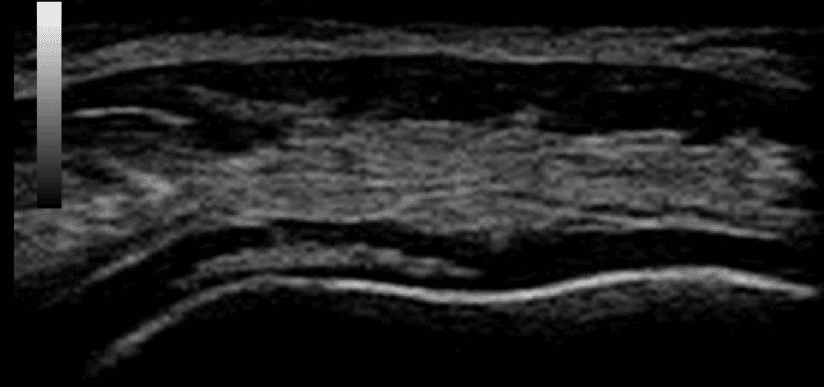
Ultrasound is useful in CPPD disease. Typically, crystal deposition is seen embedded within the substance of the hyaline cartilage in ‘rose bead’ appearance. Calcific deposits can also be seen in the triangular fibrocartilage of the wrist, menisci of the knee and tendons. It can also help in obtaining synovial fluid for an accurate diagnosis.
Figure 1: Transverse view of articular cartilage showing CPP crystals embedded within the articular cartilage ‘rose bead appearance’
References
- Clunie G et al. Oxford Handbook of Rheumatology. 4th Oxford University Press 2018.
0 Comments